Content warning: Swears and acceptance of Covid-19 as an ongoing relation in human existence.
I am both an academic and everyday anthropologist of settler society, including mostly, but not only white people. White settler supremacy conditions the societal structures and narratives we all navigate and live with. All of us, “settler” or not, are potentially complicit in upholding settler supremacy, and we can all explicitly or implicitly challenge its narratives and norms. This post is a reflection on the ways that diverse inhabitants in my fields of observation, mostly the US and increasingly Canada, either shore up or challenge dominant settler state narratives in responses to the Covid-19 pandemic and public health measures to combat it.
I’m not going to jump into the feeding frenzy around federal research grant opportunities to study Covid-19, but I thought I’d put these hypotheses out there because they’ve been slow cooking in my head since early on in the pandemic. I hope someone is researching the varied responses across settler state society, not because I think such research will curtail the pandemic, but because it’s interesting. I wish such study would help disrupt the global threat to humanity that is Covid-19 and inept governmental management of this and coming pandemics, but I don’t think that is a realistic expectation given the scripts that many settler-colonial society citizens seem intent on acting out. I am, however, happy to entertain others’ more positive projections.
As I watch the ongoing Settlerflix reality series, Covid-19: Anglo North America, now entering wave four, I discern five categories of characters in the US (and to some degree in Canada) who exhibit differing responses to the risk that Covid-19 presents at home. I don’t think the majority of the cast thinks much about global risk. Following are the five hypothesized categories, which I humorously (to me at least) abbreviate with acronyms like this is a real research project.
Hypothetical Category #1: The Conservative Privileged Risk Denialists (CPRDs)
We are all familiar with the majority white public anti-maskers—a not insignificant number of them middle-class-looking Brads and Karens—who have an affinity in the US for stars and stripes garb. In both the US and Canada, they love to waive their settler-state flags when they march on the capitols, state houses, and legislative grounds just a short walk from their gargantuan trucks and SUVs. It is not uncommon for them to have on the rear windows of their gas guzzlers that row of nuclear family stickers arranged according to gender and human/animal binaries, and also by age from parents to the youngest child, then nonhuman “pets.” Putting their families on show according to the archaic Great Chain of Being is so telling. Given the relationship of the settlers’ God to their entitlement to dominion over the land and everyone else, it is unsurprising that among them are a healthy dose of evangelical and other conservative Christians.
If this were a real research project, I would ask questions that try to get at how Covid-19 risk-related behaviour correlates with geographic location, race, Indigeneity, gender, income, and “health” status of individual interviewees. I’d craft research questions related to differences between the US and Canada in their nationalist narratives, and I’d be interested in how those narratives intersect with interviewees’ definitions of and identifications with a range of demographic categories.
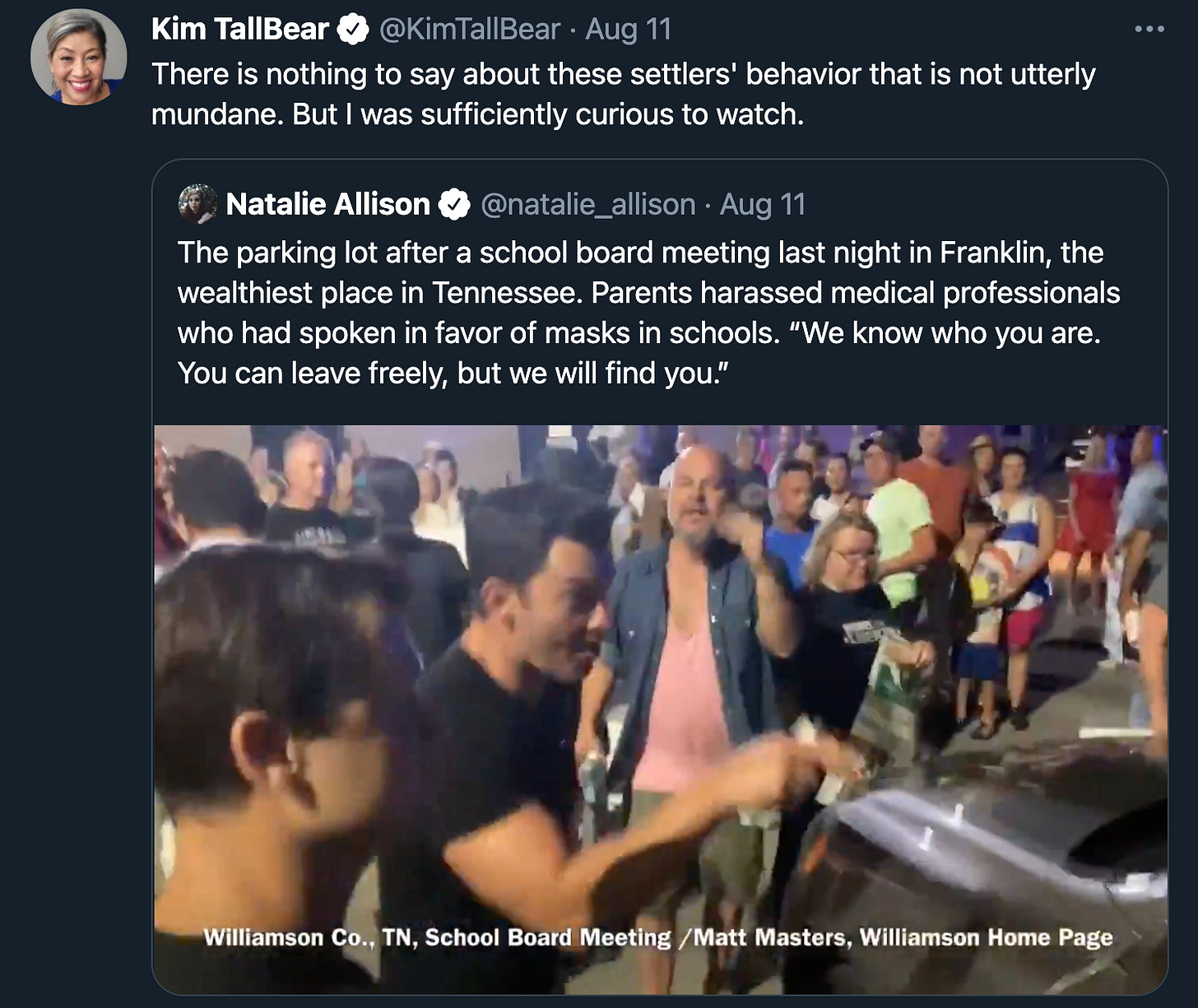
When I began drafting this post in early August, I was fascinated with a Twitter video of richer Brads and Karens at the Williamson County, Tennessee school board meeting. They were captured on camera yelling “Will not comply!” and “Fuck you!” at health care workers exiting the meeting, who had been there to advocate for mask wearing in schools. When I watch these uber-white, clean cut, some of them fresh-from-the gym-buff white people scream at and threaten medical professionals who were attempting to walk and drive away, I think of what some historians and cultural studies scholars would say. I know there is good research out there on the links between individualism, fitness, and white supremacy, so I won’t attempt that analysis. But that’s the first thing I thought of as I consumed this video multiple times.
I am interested in numbers that relate a variety of factors—geography, the urban/rural divide, religious belief, race, and income to a range of Covid risk denial activities and their varying levels of violence. I may add citational links to this post as I come across them.
Let us consider the possible pain of privileged white Tennessee parents that leads to their verbal violence and threats of future physical violence against healthcare workers in this video. My hypothesis is that these Conservative Privileged Risk Denialists (CPRDs) who comprise sometimes the wealthiest top 5% and definitely the top 10% are accustomed to living with less risk in their lives relative to the growing numbers of poor in our society. I observe that they are outraged that they are being told they and their loved-ones are at risk of becoming seriously ill and possibly dying from a viral infection, a situation that they cannot simply buy their way out of. They tell themselves and the world that these epidemics and pandemics are only supposed to be the scourge of predominantly non-white and poor countries, the inevitable destiny of those countries and peoples. If the Covid-19 scourge is real—and many of them are not convinced, as that would require recognizing USA foundational cracks or the US as unexceptional—they tell the story that there is nothing to be done about it except more capitalism and white saviourism, more “freedom.” At any rate, the deaths are almost always across the ocean blue or among non-white urbanites or on “remote” reserves and reservations. No worries, they tell themselves. They don’t much care about risk to the poor and the non-white. But they also deny their own risk and that of their children. Medical care systems are cracking under the weight of the sick and dying, and only the truly wealthy and powerful have access to high-end treatments.
Hypothetical Category #2: The Liberal Privileged Outraged at Risk (LPORs)
I don’t think I have a single CPRD friend in real life or on social media. But I have plenty of Liberal Privileged Outraged at Risk (LPOR) friends or acquaintances, many of them very highly educated. My close proximity to this second group of settler society citizens, has made me take close notice of their particular responses to Covid-19 risk.
LPORs are probably less likely than CPRDs to inhabit the top 5%, but they are almost always among the top 10%. Like CPRDS, they too are accustomed to living with far less risk in their lives relative to poor people. And like the CPRDs, they are outraged that they are being told that they and their loved-ones are at risk of becoming seriously ill and possibly dying. They are health-insured, they do yoga and eat organic. They don’t have so many co-morbidities as poor people. Their socioeconomic status and often (not always) race privilege is usually more protective.
They express more regret about wealth and race disparities for sure, but they too believe that epidemics and pandemics are unfortunately the scourge of predominantly non-white and poor communities and countries. They hope it is not simply destiny for less “developed” countries and peoples to be sicker and die sooner. They don’t always agree that more capitalism is key to saving those parts of the world, but they do often have their own brand of liberal white saviourism on offer. They tend not to use the word “freedom” as much as CPRDs. They tend to “Vote blue no matter who,” and voice more worry about risk to the poor and non-white. They are starkly different from the CPRDs on one point: they absolutely do not deny their own risk and that of their children. They recognize that the medical care systems are cracking under the weight of the sick and dying, and even more now under the gluttonous capitalists (who must be mostly Republicans, right?) who take their sustenance first. While they do still retain some ability to buy their way out of the worst of the risk, it is not nearly as much as they are used to, and they are enraged. The all-inclusive rainbow nation is failing them. In fear of newfound risk, they often retreat to their nuclear families, which offered them status, economic rewards, and more. In the pandemic, however, the immobile, quarantined, even surveilled nuclear family can be a pressure cooker. Welcome to the pain long experienced by those who did not gain privilege, but were marginalized by the norms of white settler heteropatriarchal society.
Hypothetical Category #3: The Non-Privileged Risk Fatigued (NPRFs)
I admit, most of my observations among this group are among people of colour because that’s who in my circles is most risk fatigued. I have both bougie and non-bougie family—Indigenous, Black, and POC, both biological and made kin. I have some middle-class made kin who are white. However, I don’t tend to have many poor white friends and made family, and I have no poor white kin that I actually associate with. I imagine some of my bio-relatives on my white dad’s side are probably CPRDs or NPRFs, but I am not in touch with them. The whites who I fraternize with, as indicated in the above LPOR description, tend to be more privileged and/or educated, not that all of my white acquaintances are Outraged Pandemic Karens by any means. Some of them are Relational Risk Assessors (RRAs), which I’ll describe below.
But I do have close kin who are non-white NPRFs. I have two main hypotheses formed by observing and talking to them, especially when I try to tease and cajole them into vaccinating. None of the NPRFs I know are anti-maskers; they’re not so bad at mask wearing. I will discuss the more common public perception about this group’s anti-vaccine or vaccine-hesitancy sentiments, that, I think, exist in good measure among them. But first I want to discuss the idea of risk fatigue and the risk math that can accompany their fatigue and perhaps lead to vaccine hesitancy or vaccine neglect.
To put it succinctly, poor people are at risk from so many assaults on their physical, emotional, and financial health day-in and day-out, both pre- and post-Covid, that for some, Covid-19 is just one more risk. Yes it can kill people. It is made more severe by high blood pressure, diabetes, or heart disease. But multi-generational racist trauma is killing them; poverty is killing them. Covid-19 can kill them like any unexpected disease or accident can kill them, especially in the US settler state that thinks healthcare is the privilege of the well-employed and their legal spouse or dependents. I don’t have to go on and on about this. Add Covid-19 to the gigantic multi-layered risk sandwich on the plates of the poor and under- or uninsured. Whereas LPORs might face what feels like a healthy dollop of additional risk, perhaps the poor and already severely risk-burdened judge the additional Covid-19 risk as a smaller part of their overall proportion of risk? They might want to parse their worry across the broader field of risk they live with.
I was also talking to a family member when I was home in August who noted that some Black and other people of colour say that in their communities, people are sometimes simply not accustomed to seeking preventative care in a white supremacist medical system. They go in an emergency, but have found other avenues for caring for themselves. Therefore, the white-controlled medical system’s calls for solidarity might not register, or might ring hollow. I’ll detail below my positive vaccination experience because it was an Indigenous-run vaccination clinic where I did not have to encounter anti-Indigenous sentiments and (lack of) care. There are so many questions I would ask diverse interviewees if I were going to do real research on this topic.
Finally, and in my limited personal experience of NPRFs, some do cite anti-vaccination conspiracy theories along with that explicit distrust of white-controlled medicine in the historical experiences of Black and Indigenous populations. And perhaps unlike non-expert white members of the public, they can often cite key cases/topics of bioethical violations, such as the Tuskegee Syphilis Study or forced sterilizations of Indigenous people. I get their fear: racist researchers and institutions have shown themselves to be willing and happy to experiment or perform nonconsensual medical interventions on Black people and Indigenous people, the two types of non-white bio-kin I have.
A young relative wanted me to watch a conspiracy theory video clip with them this past summer. I told my relative that their political intuition is right on, and they might want to go back to school and perhaps take a class or two related to the topic of racism in medicine; they are obviously curious and willing to spend a lot of time watching, reading, and learning. In the right place and program (although access is another serious challenge), they could get better reasoned histories. The non-white “conspiracy theorist” in the video clip my relative showed me is not wrong when he talks about white society’s lies, distortions, and biases. But he undermines his structural critique with narrative threads based on sketchy evidence.
Is it surprising when individuals who experience throughout their lives structural and individual racism, including in health “care,” and when their communities have experienced racist medical practice, scientific research, and government policies, that some among them distrust what they see as a largely white medical system and authority? On the one hand, being guarded about the truths that white “civilization” has on offer is absolutely right. We should always be skeptical of their dominant narratives as I am doing in this essay. On the other hand, we non-whites regularly take calculated risks about the bitter pills we decide to ingest from settler society, be they conceptual or material. Evidence seems sufficient to me that Covid-19 vaccines help more than they hurt, although I too am not thrilled with the colonial, racist, (hetero)sexist, and classist medical industrial complex that produces them. I, in part, distrust their motives. But I also remember that white people mostly want the vaccines, including a lot of privileged ones. And our fellow non-white planetary citizens in many other countries want them too. That might be food for thought among our non-white and otherwise non-privileged kin who are leery of the vaccine narratives of powerful whites. There are not easy decisions here for those who with good reason distrust a structurally-racist-to-the-core medical infrastructure. I am obviously not a screamer on this front. I will not call especially non-white people “stupid” or gullible who are worried about racist big pharma’s incentives to produce and distribute vaccines according to highly corporatist models that reward the richest and don’t give a shit about the poor.
Hypothetical Category #4: Stealth Vaccinators (SVs)
I expect there are individuals among the privileged risk denialists and non-privileged risk fatigued families and communities who are worried enough about Covid-19 and who are not as skeptical as their family and community members about vaccination. I suspect there is a not insignificant percentage among them who might be quietly/secretly getting vaccinated. If this were a real research project, I would have questions for them too. What information, incentives, or structural conditions (e.g. free or easier to obtain vaccines) made the difference in their (growing) vaccine acceptance? Where were they vaccinated? What was their experience? Did their decision to vaccinate sway any other family/community members? If they are partnered or coparenting with an anti-vaxxer, how are they managing that? Does having children and thinking about their risk influence their greater vaccine acceptance? What is the gender and ability disparity in broader anti-vaxxing or vaccine-hesitant communities related to those within their communities who are growing in their vaccine acceptance? Have workplace vaccine mandates made a difference? How many have weighed the pressing risk of losing a job as greater than their uncertainty about the vaccine or the virus?
Some Personal Thoughts on Risk, Rage, and Relations
Before I describe my fifth and final category of risk response to Covid-19, I have some personal thoughts on risk that help preface my explanation of that final category that I see as focused on the role of better relating to manage risk, and why I think I fall within its parameters.
Mononormativity and Covid-19 Risk
I have spent time in close proximity to risk assessment thinkers, both as an environmental policy worker in my first career, and also as a polyamorist. Somewhat akin to environmental risk assessors, those of us who mindfully practice open nonmonogamy tend to be highly risk aware and knowledgeable about risk reduction. We tend to talk openly and in an informed manner about risk tolerance for ourselves and with any potential romantic/sexual partners. We are accustomed to thinking and speaking in a measured way about risk in order to reduce it, but never with the idea that there can be zero risk.
I propose that an analysis of monogamy culture can help us also understand our ineffective societal management of Covid-19. Risky contact and denialism about the prevalence of other pathogens is already common across this mononormative society that views plural sexual relationships as ethically inferior, and privileges and conflates monogamous relationships with health and fidelity. In a mononormative society, a misperception flourishes that contracting a sexually-transmitted infection is a moral or biological failing rather than a statistically-common occurrence, especially in the absence of personal protective equipment (PPE). Such moral assumptions can hinder clear and honest conversation and negotiation of risk when mononormatives engage in sexual contact, thus making them vulnerable to infection. Common monogamist assumptions that one’s partner could not possibly be infected encourage non-regular testing and resistance to PPE, e.g. condoms.
I see failure narratives related to infection also shaping societal responses to Covid-19, and resistance not only to PPE, but to physical distancing guidelines. “All those safety practices are not necessary for moral and healthy subjects who are obviously less likely to be infectious, right?!” Unfortunately, we see these infection-as-failure narratives even among seemingly more rational societal actors like the Liberal Privileged Outraged at Risk. Perhaps a mononormative society is less intellectually and socially equipped to deal thoughtfully with risk of infection?
Why Not Rage?
Due probably to a combination of my risk assessment orientations and my age—where once angry conflagrations have burned into weary embers—I have not become pandemic outraged. My relative privilege and ability to both physically and emotionally distance at this later stage of life is also key. But given how many similarly privileged people I see being outraged, I also think my lack of rage is due to the fact that I grew up with far less privilege; I was not conditioned to expect distance from disaster. As a child and young adult, I lived in wait of the next crisis and developed a flight response to stay a step ahead of impending storms. Stopping fleeing has been a formidable life project. I have commiserated with a colleague in my Faculty of Native Studies that because we grew up in economically unstable Indigenous communities under colonial assault, we never feel quite safe. Formative years cut deep despite our current privileges compared to many of our relatives.
I also cannot find outrage because I am totally unsurprised by seemingly “irrational” risk behaviours exhibited around this contagion. I’ve noted, for example, the risk denial and associated outrage of some privileged people. I’ve also noted that some who are less privileged weigh Covid-19 risk more lightly against their histories and scars of medical racism and other daily dangers. I don’t think either response, though I judge the first more harshly than the second, is actually irrational. Both are responses, though fundamentally different in positionality and experience, to the failures of the settler state and its core exceptionalist narratives.
Like the Non-Privileged Risk Fatigued (some of whom are my relatives), I retain some risk weariness and trauma from my earlier life, while it doesn’t translate into deep skepticism about the efficacy of vaccines. I am deeply skeptical of the motives of pharmaceutical companies that seek profit first and foremost and perform their medical experimentation and drug trials in a geopolitically-, race-, and class-stratified world.
Throughout the pandemic, I’ve weighed personal risk and interests in relation to collective risk and interests. Given that I work at home, mostly live alone, and had already survived a bout of Covid-19 without much apparent problem, I did not rush to get vaccinated when Canada did early rollout of vaccines to a statistically-vulnerable Indigenous population in late winter and spring of 2021. I believe that we should put the most vulnerable first. At the same time, my knowledge of racist medicine led me to be a little skeptical on my own behalf. I wanted to observe vaccine side effects across the population, but I was also pretty sure that they provide more benefit than risk for most people. My willingness to wait was due then to both individual and collective risk calculations and interplay.
Better Relations at the Indigenous Vaccine Clinic
I am a person raised in Indigenous communities, both urban and reservation. That life experience developed in me a sense of obligation to Indigenous collective well-being. This commitment figured prominently in my decision at first not to go to the Métis Nation of Alberta (MNA) vaccine clinic in March of this year ahead of my eligibility-by-age in Alberta. My reasons had to do with not only my perceived level of vulnerability to Covid-19, but also my respect for geographic-specific definitions of Indigeneity. Since I am from the US side of the border, I am not officially identified as “Métis, First Nation, or Inuit,” the Indigenous categories specified on the MNA website as eligible for vaccination. I felt that those who are Métis, First Nation, or Inuit and who are at greater risk for a variety of reasons should go ahead of me.
I did, however, end up being vaccinated by the MNA as part of that initiative. An Indigenous healthcare worker acquaintance of mine informed me that there were appointments available and they would be happy to vaccinate me if I explained that I was a tribal citizen in the US and a resident of Alberta. At that person’s insistence, I went to the vaccination centre; it was one of the most pleasant medical experiences I’ve had. I was required to show my Alberta health card, but not my tribal ID, which I had on me just in case. The Métis cultural scene was integrated into a congenial and efficient vaccination clinic. We were given MNA swag (e.g a cute Métis sash design lanyard) and the post-vaccination waiting area was populated with Indigenous people my age and older. We watched a video of fiddling and jigging while we waited the post-vaccination requisite 15 minutes for the possible rare allergic reaction. I was delighted by the whole scene, as much by the Indigenous-centric healthcare delivery as by the thought of getting vaccinated. I need to emphasize the fact that self-identification as Indigenous was acceptable at the vaccine clinic. This is inclusionary for Indigenous people who for various reasons do not have official status as Indigenous, the upside to allowing for self-identification. The downside to self-identification, is it opens the door to fraudulent claims to being Indigenous to gain resources meant for Indigenous peoples, including early vaccine access.
I wonder if my vaccine-hesitant family members would have been vaccinated sooner if they were living on our reservation where there would be: 1) Indigenous community pressure to vaccinate; 2) more regular contact with more family members, some of whom are more vulnerable; and 3) if they could obtain vaccines from our tribally-controlled clinic. My vaccine-hesitant relatives live in urban areas. Vaccination is a cultural experience no matter where you do it, and not every venue is very comfortable or feels safe for populations who have been the object of medical racism for centuries. A history of bad relations matters as does the active presence of better relations.
Hypothetical Category #5: Relational Risk Assessors (RRAs)?
This final category of societal risk response is the one I see myself falling into, but with a healthy dose of cynicism about the possibility for good societal risk relations. I see relational risk assessment as characterized by:
1) considered attention to individual and structural risk, both historically and today; including
2) the idea that individual and collective risk (or lack of it) are co-constitutive—that they shape and facilitate one another in the moment and over time and space; and
3) an attention to learning individual and collective risk reduction strategies that help mitigate risk for the most vulnerable.
My understanding of relational risk assessment is not derived from some kind of universal emotional or spiritual love for all of humankind, but is more rooted in the materiality of my own past deprivations and exposures to suffering. I don’t want others to suffer as much, or in many cases far worse, than I, my family, and People have suffered. My material or physical aversion to my suffering and the suffering of others is linked, of course, to my profound regard for the specialness of this planet as a whole, even if I do not experience universal human love. I understand that my individual risk is entangled with collective risks. And I understand that the risks to persons and Peoples I do love are entangled with risks to other persons and populations across the globe, including both human and other-than-human persons. All of our fates are entangled.
In her May 2020 essay, “The Virus is a Relation,” non-Indigenous, feminist philosopher Alexis Shotwell explains what I think of as “relationally-constituted risk”:
Whether people live or die when they get sick depends on webs of social relations, the history of oppression carried in their bodies, what care is made available for them to receive, and so much that we don’t yet understand.
Shotwell also calls attention to the bad treatment by some humans of other-than-humans—what we can call “ecological” relations.
I read closely Shotwell’s caution regarding policing the virus as something that can be “kept out of a country, neighborhood, or body.” Shotwell suggests instead “that when people move from thinking about their own body boundaries as a domain they need to seal off and protect from viral intrusion and start thinking about their practices in terms of trying to not transmit the virus to the people they encounter, their activities change.” Masking, Shotwell explains, becomes about protecting others; staying home if possible is an act of generosity, not selfishness.
Beyond individual acts directed toward community care, Alexis Shotwell emphasizes the structural conditions that support Covid-19’s dangerous circulation in the human population: capitalist modes of consumption that make housing a commodity instead of a right, the nuclear family organized around the couple, and the organization of care around those unsustainable units. This kind of system leaves many vulnerable to deprivation and violence. Finally, Shotwell asks even as we consider the benefits to the earth of the temporary disruption to fossil fuel consumption brought by Covid-19, that we not succumb to the “heartless rhetorical move” that all of this death is some kind of universal retribution. Instead, we might consider a narrative of living with: “What relationship with this virus will proliferate survivance and flourishing, now and later?”
I have pondered Alexis Shotwell’s careful essay each time I’ve read it over the past 17 months. Yet I do not claim that my individual version of relational risk behaviour is as heart-generous as I know Shotwell’s to be. I am structurally caring and supportive. I believe as a society that we should house, feed, and provide care for our relations. But I also don’t want to be out circulating among all of my societal relations. I am prone to containment on a personal level primarily for social reasons. I prefer staying home and away from most humans. I need space, order, and quiet. Me staying home is very much about my personal aversion to overwhelming social contact. Lucky me, my self-interest in this instance also reduces Covid-19 risk for others. I want to be clear about this, because I don’t want to present myself as some kind of good Samaritan that I am not.
It is also true that I have been more concerned with not putting others at physical risk from Covid-19 than I have been concerned with not putting myself at risk of the virus, although I don’t put myself at risk for insignificant reasons. When I took my biggest Covid-19 risk during this pandemic, it involved both cold calculation—an informed knowledge of what I was risking, and an emotional need to see my loved one who I missed terribly, not having seen them in months due to Covid-19 border restrictions. So I traveled to the US from Canada and cohabited for a month with that person, a frontline worker, who was at serious risk. I also knew that if they stayed where they were, living with another vulnerable and immune-compromised person, that medically vulnerable person could instead catch Covid-19, and have a good chance of dying. I wanted my loved one with me and I also didn’t want them to live with the guilt. I thought I would likely come through the infection okay since I have rarely been sick in my life. I did indeed contract Covid-19. Luckily, my gamble paid off and I came through it okay as far as I can tell. Would I have done that if I were an immune-compromised person and I feared I might seriously risk my life? Nope.
We might be relational risk assessors in a variety of ways.
Future Scenarios?
I stayed up until 2 a.m. watching the zombie series Black Summer one night in August when I began drafting this post. This is why I will usually only watch films, not series. I binge on zombies; a film involves only moderate consumption of those usually predictable narratives of mostly settler society gratuitous violence and non-cooperation. I was asking myself when I finally finished the series and went to bed disgusted: “Would people REALLY BEHAVE LIKE THAT? I mean, why not cooperate?! Place your best few shooters at lookout points. Don’t let a random zombie just run around screaming for days, then send one of your guys out for wood with the zombie on the loose. While the shooters keep an eye on the property’s periphery, the rest of the humans cooperate to fortify the building they’re sheltering in. Why descend into suspicious, selfish chaos and….” LOL. Oh my god, what was I thinking? There was a point when it looked like the women in Black Summer would be the last standing humans, and I had a glimmer of hope that the pointless He-Man responses would cease, but then all but two of the women got shot and/or turned.
This Indigenous anthropologist of all things settler has no zombie apocalypse to observe. I’ll watch instead the settler supremacist civilization’s response to Covid-19. As a zombie film aficionado, I could hypothesize a possible sensationalist conclusion to Covid-19: Anglo North America, but I don’t want to carry the tongue-in-cheek too far. As for hypothesizing “more realistic” future scenarios, that will require sustained research across multiple fields: history of science and medicine, global and public health, epidemiology, critical race studies, political ecology, futurism studies, and many more areas of inquiry. I can’t quite say I’ll look forward to the reading, although I promise to be fascinated if I am still alive and capable of processing the insights; I am a “recovered” Covid-19’er, after all, with perhaps a viral time bomb in my brain.
Thank you as always for reading and/or listening.












Share this post